Embryo Transfer is never one size fits all. The options can be confusing and in this blog, we discuss what a frozen vs fresh embryo transfer may imply.
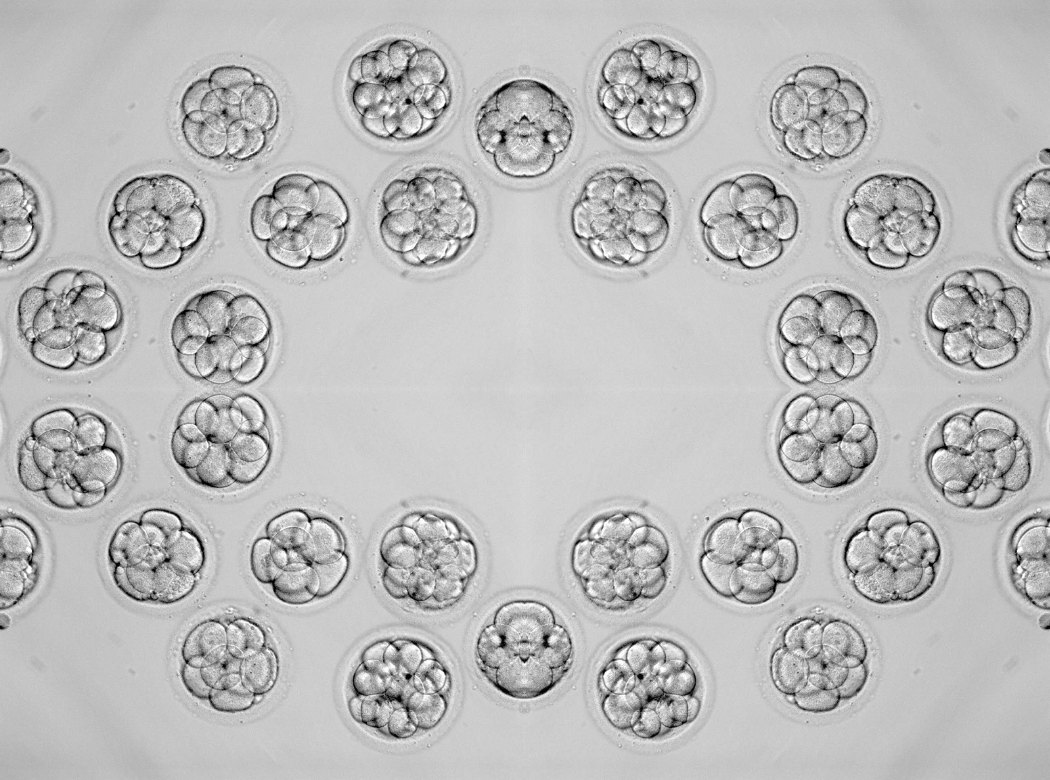
You’ve made it through stimulation and egg retrieval. Your embryos are developing beautifully. And now your doctor tells you: we’re doing a freeze-all cycle, or we’re planning a fresh transfer.
You might be wondering—what’s the difference? Why one over the other? Let’s break down what each option means and what drives this medical decision.
What's the Difference?
Fresh embryo transfer: Your embryos develop for about 3-5 days after retrieval, then the best one(s) are transferred directly into your uterus in the same cycle.
Frozen embryo transfer (FET): Your embryos are developed over 3-5 days just like in the fresh cycle, but here they are then frozen or cryopreserved in liquid nitrogen. The embryo transfer is typically done in a later cycle. When ready, the embryo is thawed (brought to a specific temperature) and then transferred.
The only difference is timing and whether the embryo goes through a freeze-thaw cycle.

Why Frozen Transfers Have Become More Common
Frozen transfers now account for over 50% of all IVF transfers. Why?
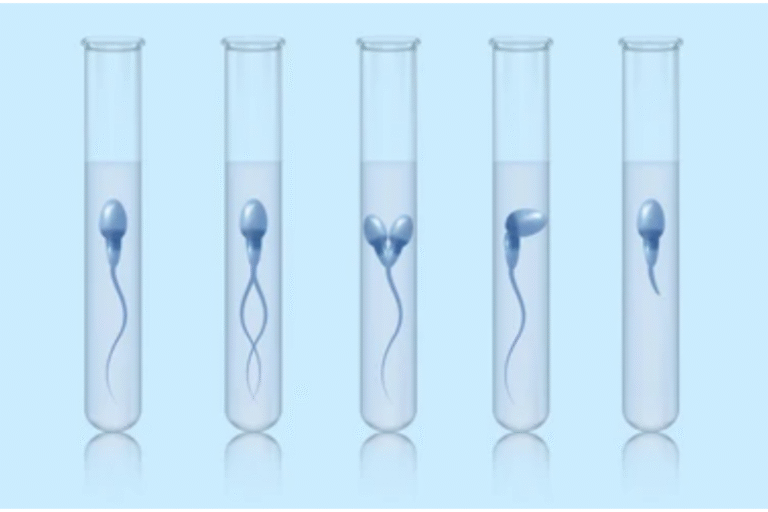
Better freezing technology: Modern vitrification has 95-99% embryo survival rates.
Genetic testing: PGT-A requires freezing while waiting for results.
Optimizing endometrial receptivity: The main advantage of frozen transfer is giving your uterus the best possible environment for implantation.
When Your Doctor Recommends Fresh Transfer
You want results faster: Fresh means potential pregnancy 2-3 weeks after retrieval. Frozen adds 1-2 months to your timeline.
Lower upfront costs: Avoids freezing, storage, and thawing fees, making it more economical.
Your cycle looks ideal: Low to normal stimulation response, progesterone levels under 1.5 ng/ml at trigger, and thick, well-developed endometrial lining (8mm or more). When everything lines up perfectly, fresh transfer works beautifully.
Very few embryos: With only 1-2 embryos, your doctor might recommend fresh to avoid any (tiny) risk of embryos not surviving the freeze-thaw process.
Normal ovarian reserve with good response: When your cycle isn’t hyperstimulated and hormones aren’t excessively elevated, your body can handle both egg production and optimal endometrial preparation simultaneously.
When Your Doctor Recommends Frozen Transfer
High risk of OHSS: If estrogen or progesterone is very high or you have many follicles (typically >20), freezing eliminates the risk of ovarian hyperstimulation syndrome worsening with pregnancy. OHSS can be dangerous, and pregnancy makes it worse, so freeze-all is the safest option.
Elevated progesterone at trigger: Progesterone >1.5 ng/ml at trigger is associated with 20-30% reduced fresh transfer success due to endometrial advancement. Freezing and transferring in an unaffected cycle significantly improves outcomes.
Thin endometrium during stimulation: If your lining isn’t optimal (under 7mm) despite stimulation, you can build it more effectively in a frozen cycle with focused endometrial preparation protocols.
You produced many embryos: High response (>15-20 eggs) suggests elevated hormones that might affect receptivity. Your ovaries did their job beautifully, but your uterus needs recovery time.
You want genetic testing: PGT-A requires freezing embryos for 1-2 weeks while awaiting results. This gives you information about chromosomal normalcy before transfer.
Previous failed fresh transfer with good embryos: If you’ve had high-quality embryos that didn’t implant in a fresh cycle, frozen transfer might optimize your endometrial environment.
Personal or medical timing needs: Surgery needed, illness, travel, or just needing a break emotionally or physically before transfer.
Success Rates: What the Data Shows
Recent studies show that frozen transfers often have equal or slightly better outcomes than fresh transfers, especially when fresh cycles involve elevated hormones or high stimulation.
For women with normal responses and optimal hormone levels, success rates are similar—around 44-47% for both fresh and frozen. But when progesterone elevation or hyperstimulation occurs, frozen transfer offers clear advantages by allowing your endometrium to recover and be optimally prepared.
Our Approach
We individualize based on:
- Hormone levels at trigger (especially progesterone and estrogen)
- Number of follicles and OHSS risk
- Endometrial thickness and quality during stimulation
- Whether you want genetic testing
- Your previous cycle history
- Your personal timeline and preferences
We monitor progesterone levels carefully. If they’re elevated at trigger, we typically recommend freeze-all to give your endometrium optimal conditions. If your cycle is well-controlled with normal hormone levels and good lining, fresh transfer works beautifully.
If you’re deciding between fresh and frozen transfer, let’s discuss your options. We’ll review your hormone levels, cycle response, and endometrial quality to help you make an informed choice.
Book a consultation to create a personalized transfer plan.
Because the decision about when to transfer should be based on your body’s response—not a one-size-fits-all protocol.