A quick look at the menstrual cycle and what is actually happening when you’re trying to get pregnant.
If you’re trying to conceive, understanding your menstrual cycle is essential. But most of us weren’t taught much beyond “you get your period once a month.” The reality involves a carefully timed dance of hormones that prepares your body for pregnancy each month.
Let’s break down what’s actually happening and why it matters for getting pregnant.
The Big Picture: Two Cycles Working Together
Your menstrual cycle is actually two cycles at once:
The ovarian cycle: What’s happening in your ovaries—follicles growing, egg release, and transformation afterward.
The uterine cycle: What’s happening to your uterine lining—shedding, rebuilding, and preparing for pregnancy.
These are controlled by hormones from your brain and ovaries, talking to each other constantly. A typical cycle is 21-35 days (28 days average). Day 1 is the first day of full menstrual flow.

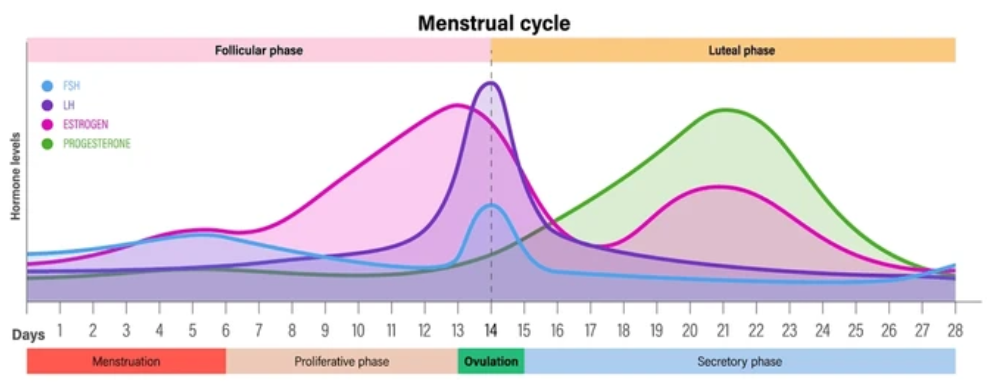
The Four Key Hormones
FSH (Follicle-Stimulating Hormone): From your brain, tells your ovaries to grow follicles (tiny sacs containing eggs). The “start” signal.
LH (Luteinizing Hormone): Also from your brain, triggers egg release. The “go” signal.
Estrogen: Made by growing follicles. Builds up your uterine lining.
Progesterone: Made after ovulation. Prepares and maintains the lining for pregnancy.
The Four Phases
Phase 1: Menstruation (Days 1-5)
In your ovaries: The previous cycle has ended. Progesterone drops, triggering your period.
In your uterus: The lining sheds because there’s no pregnancy. This is your period—blood, tissue, and the unfertilized egg.
Hormones: Estrogen and progesterone are at their lowest. FSH starts rising, signaling your ovaries to grow new follicles.
Fertility: Not fertile now, but preparation for your next fertile window is starting.
Phase 2: Follicular Phase (Days 1-13)
In your ovaries: Rising FSH makes several follicles (5-10) start growing. Around day 7, one becomes the “dominant” follicle and grows fastest. Why only one? It produces more estrogen, which tells your brain to reduce FSH. Lower FSH starves the smaller follicles. The dominant follicle survives because it has extra FSH receptors.
In your uterus: Rising estrogen tells the lining to rebuild and thicken—from about 2-4mm after your period to 8-12mm by ovulation. Blood vessels multiply and glands develop.
Hormones: FSH rises, then levels off. Estrogen rises steadily as the dominant follicle grows.
Fertility: You’re approaching your fertile window. The last 3-5 days of this phase are when fertility begins.
The lesser-known truth: This phase varies in length (10-23 days) between women and even between your own cycles. This is why cycle lengths differ—the follicular phase changes, but the next phase stays consistent.
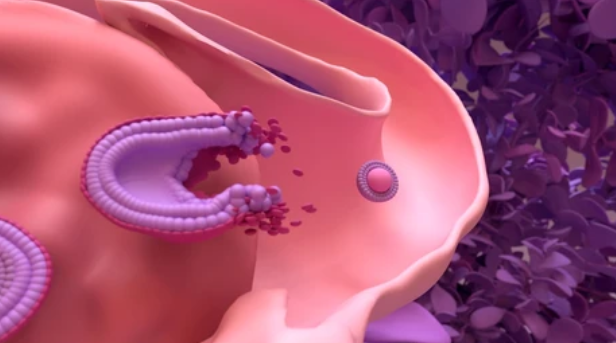
Phase 3: Ovulation (Around Day 14, but varies)
What triggers it: When estrogen reaches a critical high level, it switches from suppressing LH to triggering a massive LH surge. This surge lasts 24-48 hours. Ovulation predictor kits detect this surge.
In your ovaries: The LH surge causes the mature egg to finish developing, weakens the follicle wall, and triggers its rupture. The egg is released into the fallopian tube. This happens 28-36 hours after the LH surge begins.
In your uterus: The lining is thick, lush, and ready. Estrogen drops right after ovulation as the follicle collapses.
Fertility: Your most fertile time. The egg survives 12-24 hours after release. Sperm can survive 3-5 days in fertile mucus. Your fertile window is roughly 5 days before ovulation plus ovulation day.
Signs: Some women notice mid-cycle cramping, clear stretchy cervical mucus (like egg white), increased sex drive, slight temperature rise, or breast tenderness.
Phase 4: Luteal Phase (Days 15-28)
In your ovaries: The ruptured follicle transforms into the corpus luteum—a temporary structure that produces lots of progesterone and some estrogen.
In your uterus: Progesterone transforms the lining into a secretory, nutrient-rich environment. The lining becomes thick and spongy, full of blood vessels and glands packed with nutrients for a potential embryo.
If pregnancy happens: An embryo implants around days 20-24 (6-10 days after ovulation). It produces hCG, which tells the corpus luteum to keep making progesterone. The corpus luteum sustains pregnancy until about 10 weeks, when the placenta takes over.
If no pregnancy: Without hCG, the corpus luteum dies after 12-14 days. Progesterone and estrogen drop. This triggers blood vessels to constrict, cutting off blood supply. The lining breaks down and sheds—your period starts. Day 1 of your next cycle.
Hormones: Progesterone dominates, peaking around day 21. Both hormones suppress FSH and LH.
Fertility: Not fertile—ovulation already happened.
Length: Very consistent—12-16 days (usually 14) for most women, unlike the variable follicular phase.
Why Understanding Your Cycle Matters
Timing sex: Knowing when you ovulate helps you time intercourse during your fertile window—when pregnancy is actually possible.
Identifying problems: Irregular cycles, very short or long cycles, or missing periods signal potential issues needing evaluation.
Confirming ovulation: If you don’t ovulate regularly, you can’t conceive. Understanding your cycle helps track ovulation.
Fertility testing: Hormone tests are done on specific days because levels change dramatically. FSH/estrogen on days 2-5. Progesterone around day 21 to confirm ovulation.
Pregnancy testing: Understanding the luteal phase helps you know when to test (after a missed period) and when implantation occurs.
When Your Cycle Signals a Problem
No period: Probably not ovulating. Needs evaluation.
Very irregular cycles: Suggests inconsistent or absent ovulation. Common with PCOS.
Very short cycles (under 21 days): May mean poor egg quality or short luteal phase.
Very long cycles (over 35 days): Often means delayed or absent ovulation.
Very heavy bleeding: May indicate fibroids, polyps, or hormonal issues.
Spotting between periods: Can signal hormonal imbalance or structural issues.
If you’re under 35 and trying for 12 months, or over 35 and trying for 6 months without success, see a fertility specialist—even if cycles seem normal.
Ready to Understand Your Fertility Better?
Your menstrual cycle is your body’s monthly preparation for pregnancy. It’s driven by hormones talking between your brain and ovaries, with your uterus responding by building and shedding its lining.
Understanding these phases helps you identify your fertile window, recognize problems, and work effectively with your doctor if needed.
Your cycle is one of your body’s most reliable indicators of reproductive health.
If you’re tracking your cycle and have questions, experiencing irregular periods, or trying without success, let’s talk. We can evaluate your cycle, identify issues, and help optimize your chances.
Book a consultation to discuss your menstrual cycle and fertility concerns.
Because understanding your body is the first step toward building your family.