Sexually transmitted infections affect fertility pretty significantly. This post breaks it down for you.
Your doctor just mentioned ICSI during your IVF discussion, and now you’re confused. Isn’t IVF already complicated enough? Why are there different types? And how do you know which one you need?
Let’s break down the difference between conventional IVF and ICSI in simple terms, so you understand exactly what’s happening with your eggs and sperm—and why your doctor might recommend one over the other.
The Basic Difference
IVF: Eggs and sperm are put together in a dish and fertilization happens naturally—the sperm swim to the eggs, penetrate on their own, and fertilize them.
ICSI: A single sperm is picked up with a tiny needle and injected directly into each egg by an embryologist.
That’s it. Everything else about the IVF process—stimulation, egg retrieval, embryo culture, transfer—is exactly the same. The only difference is how the egg and sperm meet.
How Conventional IVF Works
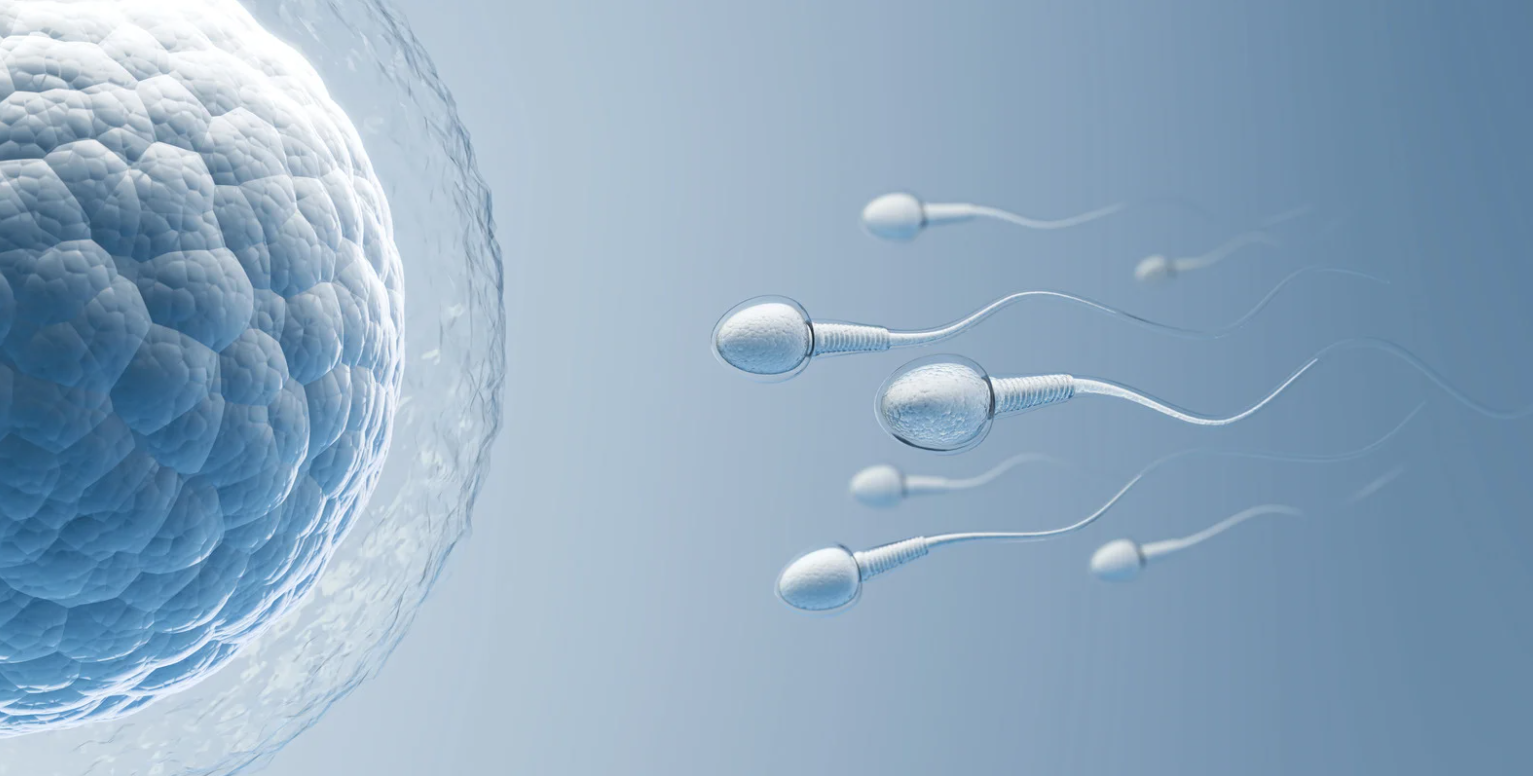
In conventional IVF (often just called “IVF”), after your eggs are retrieved, they’re placed in a culture dish with tens of thousands of sperm. The sperm swim around, find the eggs, bind to the egg’s outer layer (the zona pellucida), and penetrate it to fertilize the egg—just like what would happen naturally in your fallopian tube, except it’s happening in a lab dish.
This mimics natural fertilization as closely as possible. The strongest, healthiest sperm naturally win the race and fertilize the egg.
When conventional IVF works well: When sperm count, motility (movement), and morphology (shape) are normal or near-normal, conventional IVF usually works beautifully. About 50-66% of eggs typically fertilize this way.
How ICSI Works
In ICSI (Intracytoplasmic Sperm Injection), an embryologist uses a microscope and very fine tools to:
- Select a single sperm that looks healthy
- Immobilize it (by gently crushing its tail)
- Load it into a glass needle thinner than a human hair
- Pierce the egg’s outer layer
- Inject the sperm directly into the egg’s center
ICSI was developed in the 1990s specifically for severe male factor infertility—cases where sperm couldn’t fertilize eggs on their own. It revolutionized treatment for men with very low sperm counts or poor sperm quality.
ICSI fertilization rates: About 50-80% of eggs injected with ICSI fertilize successfully.

When ICSI Is Clearly Needed
ICSI is the right choice when:
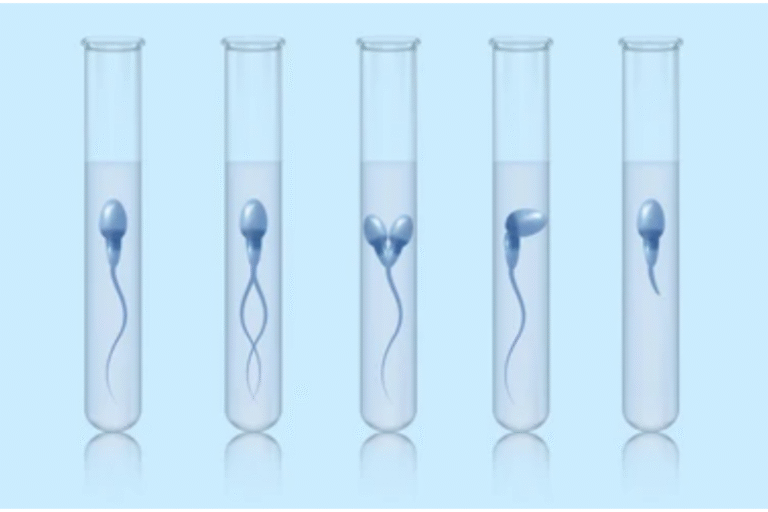
Severe male factor infertility: Very low sperm count (under 5-10 million/ml), very poor motility (most sperm don’t move), or very abnormal morphology (fewer than 4% normal-shaped sperm).
No sperm in the ejaculate: If sperm needs to be surgically retrieved from the testicles or epididymis (due to vasectomy, blockage, or other issues), ICSI is required because there aren’t enough sperm for conventional IVF.
Previous fertilization failure: If you’ve done conventional IVF before and no eggs fertilized (or very few did), ICSI prevents that from happening again.
Very few eggs retrieved: When you only have 1-3 eggs, ICSI maximizes the chance that each egg will fertilize.
Using frozen sperm: Frozen sperm don’t always swim as well as fresh sperm, so ICSI ensures fertilization.
PGT testing: Some clinics prefer ICSI when doing genetic testing of embryos to avoid contamination from extra sperm that might stick to the egg.
In these situations, ICSI isn’t optional—it’s necessary.
So Which Should You Choose?
Choose ICSI if:
- You have severe male factor infertility (very low count, poor motility, abnormal morphology)
- Sperm was surgically retrieved
- You’ve had total or very poor fertilization with conventional IVF before
- You have very few eggs (1-3)
- You’re using frozen sperm
- Your doctor has specific concerns about fertilization potential
Choose conventional IVF if:
- Sperm parameters are normal or mildly abnormal
- You have no history of fertilization failure
- You’re doing your first IVF cycle with reasonable sperm quality
- You want to maximize live birth rates (based on recent research)
Hybrid approach: Some clinics do “split ICSI”—they use conventional IVF on half your eggs and ICSI on the other half. This provides a safety net if conventional IVF doesn’t work, while still giving you the benefits of natural selection.

Our Approach
We don’t use ICSI routinely for everyone. We use it when there’s a clear medical indication—male factor infertility, previous fertilization failure, very few eggs, or surgically retrieved sperm.
If you’re on the fence, we can discuss a split approach—using both methods on different portions of your eggs to see how each performs.
If you’re about to start IVF and wondering whether you need ICSI, let’s have an honest conversation. We’ll review your partner’s semen analysis, your history, and help you make an evidence-based decision about which fertilization method gives you the best chance of success.
Book a consultation to discuss your personalized IVF plan, including whether ICSI makes sense for your unique situation.