PRP is a relatively new treatment for ovarian and endometrial rejuvenation. Here we take a deep dive into what it is and if it actually works.
Platelet-Rich Plasma, or PRP, has been called “liquid gold” in fertility circles. You’ve probably seen it mentioned online—your own blood, concentrated and injected back into your ovaries or uterus with the promise of rejuvenation. It sounds almost magical.
But does it actually work? And more importantly, is it right for you?
What Is PRP, Actually?
PRP stands for Platelet-Rich Plasma. Here’s the simple version:
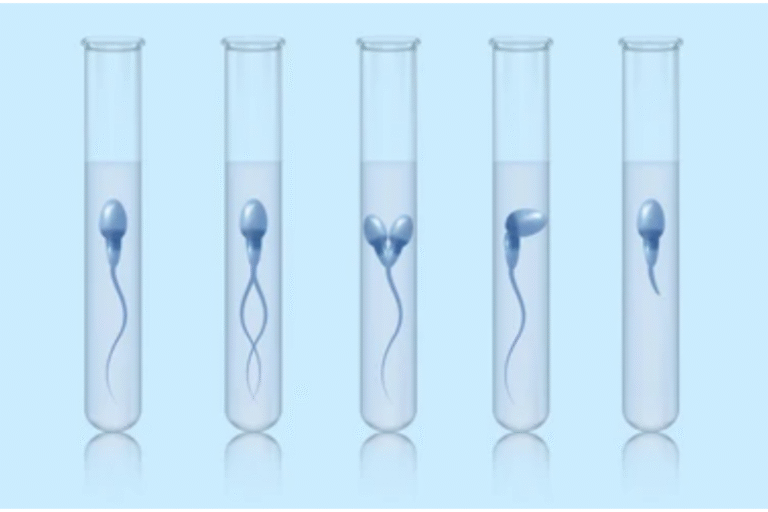
We draw a small amount of your blood, spin it in a centrifuge to separate the components, and collect the plasma that’s now concentrated with platelets—those tiny cell fragments packed with growth factors that help heal and regenerate tissue.
This concentrated plasma is then injected either:
- Into your ovaries to potentially stimulate follicles and improve egg quality
- Into your uterus to thicken the endometrial lining and improve implantation
Those growth factors will stimulate tissue regeneration, improve blood flow, and essentially “rejuvenate” your reproductive organs.

PRP for Ovaries: What Does the Research Say?
The promise: Wake up sleeping follicles, improve egg quality, give women with poor ovarian reserve a chance to use their own eggs.
The reality: Studies on ovarian PRP have shown mixed results.
Early research looked encouraging—some women’s hormone levels improved, and a few achieved spontaneous pregnancies. More recent randomized controlled trials, however, have given us varied outcomes. Some studies showed improvements in eggs retrieved but not in pregnancy rates, while others found minimal differences between women who received PRP and those who didn’t.
The honest take: Studies on ovarian PRP show mixed results. Some women seem to benefit, while others don’t see improvements. The research is still evolving, and we’re learning more about which patients might respond best.
What this means for you: Ovarian PRP may be useful in specific cases, but treatment needs to be individualized. Your response depends on factors like your age, ovarian reserve, and overall fertility picture. This is definitely something to discuss thoroughly with your doctor.
PRP for Endometrium: A More Promising Story
Now here’s where things get better. PRP for thin endometrium actually has decent evidence behind it.
The problem it addresses: Some women have persistently thin uterine lining (less than 7mm), which makes implantation difficult. This can happen after D&Cs, with scar tissue, or sometimes for unknown reasons. Standard treatments don’t always work.
What the research shows: Multiple studies—including some good randomized trials—have found that PRP infusion into the uterus can increase endometrial thickness and improve pregnancy rates in women with thin lining.
Why might it work for endometrium but not ovaries?
The endometrium naturally regenerates every month—it’s designed to grow and shed. Ovaries? Not so much. Once follicles are depleted or eggs have aged, bringing them back to life is much harder. The endometrium is simply more responsive to regenerative treatments.
The honest take: If you have a persistently thin lining that hasn’t responded to everything else, PRP is worth considering. It’s not guaranteed, but there’s reasonable evidence it can help.

Who Might Consider PRP?
Based on current research, here’s a helpful framework:
PRP for endometrium may help if:
- You have persistently thin lining (less than 7mm) despite standard treatments
- You’re facing cycle cancellation because your lining won’t grow
- You have recurrent implantation failure with thin lining
- Standard options haven’t worked and you need another approach to try
PRP for ovaries might be discussed if:
- You have diminished ovarian reserve and want to explore all options
- Standard stimulation protocols haven’t yielded good results
- You’re looking for additional approaches before considering donor eggs
- You understand that results vary and want to try it as part of a comprehensive plan
Important note: Whether PRP is right for you depends entirely on your individual situation. Studies show mixed results, which means some patients benefit while others don’t. The best way forward is an honest discussion with your fertility specialist about your specific case, what the evidence shows, and what realistic expectations look like for your circumstances.
Our Approach to PRP
We offer PRP treatments at our clinic, but we believe in being completely transparent about what it can and cannot do.
For endometrial PRP: We recommend it for specific patients—those with thin lining who haven’t responded to standard treatments. We’ve seen it help women who were facing cycle cancellation or considering surrogacy. It’s not a miracle cure, but it’s a reasonable option when other approaches have failed.
For ovarian PRP: We’re honest that the evidence is weak. We don’t lead with it or present it as proven. If you’ve exhausted other options and want to try it understanding it’s experimental, we can discuss it. But we won’t sell you hope without science to back it up.
Ready to Discuss Whether PRP Is Right for You?
If you’re dealing with thin endometrium, recurrent implantation failure, or poor ovarian reserve and wondering whether PRP could help, let’s talk. We offer PRP treatments at our clinic, but more importantly, we offer honest conversations about whether it makes sense for your specific situation.
Book a consultation with us to review your case, discuss what the evidence actually shows, and create a treatment plan based on science, not hype.
Because you deserve a clinic that will tell you the truth—even when the truth is “we’re not sure yet” or “let’s try something with better evidence first.”