Semen Analysis is an integral part of fertility work up and yet most people don’t know what it tells us.. and what it doesn’t.
If you’re struggling to conceive, one of the first tests your doctor will order is a semen analysis. It’s simple, non-invasive, and gives crucial information about male fertility. Yet it’s also one of the most misunderstood tests in fertility medicine.
Let’s break down exactly what this test measures, what those numbers mean, and—just as importantly—what it cannot tell you.
What Is a Semen Analysis?
A semen analysis evaluates both the quantity and quality of sperm in a semen sample. The test looks at multiple factors that help determine whether sperm can successfully fertilize an egg.
The sample is collected through masturbation after 2-7 days of no ejaculation. This waiting period matters—too short and counts may be low; too long and movement can decrease. The sample should be tested within 30-60 minutes of collection for accurate results.
What the Test Measures
Volume (1.4 ml or more is normal)
The total amount of semen. Low volume might mean a collection problem, incomplete sample, or issues with seminal vesicles or prostate. Very high volume can dilute sperm.
Sperm Concentration (16 million/ml or more)
How many sperm are in each milliliter. This is “sperm count.” The total count (concentration × volume) should be 39 million or more per ejaculate.
Total Motility (42% or more)
What percentage of sperm are moving at all—swimming forward, swimming in circles, or just wiggling. Movement matters because sperm need to swim through the female tract to reach the egg.
Progressive Motility (30% or more)
The more important measure—what percentage are swimming forward in a relatively straight line. These have the best chance of reaching and fertilizing an egg.
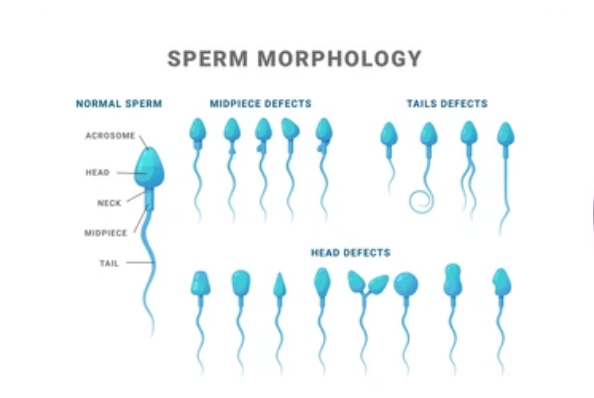
Morphology (4% or more normal forms)
What percentage have a normal shape (normal head, neck, and tail). Even fertile men typically have only 4-15% normally shaped sperm. This is the most subjective measurement and can vary between labs.
Vitality (54% or more alive)
When movement is very low, this test shows whether sperm are dead or alive but unable to move. It helps explain why motility is poor.
White Blood Cells (fewer than 1 million/ml)
High white blood cells can mean infection or inflammation, which can affect sperm quality.
pH (7.2 or higher)
Measures acidity/alkalinity. Abnormal pH can suggest infection or problems with seminal vesicle or prostate.
Liquefaction
Semen starts thick and gel-like, then should become liquid within 20-30 minutes. Poor liquefaction can affect sperm movement.
Understanding the Normal Values
The numbers above come from the World Health Organization’s 2021 guidelines—the current global standard. These values are based on men who achieved pregnancy within 12 months.
The lesser-known truth: These are lower limits, not pass/fail cutoffs. Many men with values below these can still father children naturally, and some men with “normal” values may still have fertility issues. The test gives information, not a definitive diagnosis.
What Semen Analysis Tells Us
Sperm production: Whether the testicles are producing adequate numbers.
Movement ability: Whether sperm can move well enough to reach an egg.
Basic structure: Whether sperm are shaped normally enough to function.
Male factor issues: If results are abnormal, male infertility is likely contributing to conception problems.
Treatment direction: Results help determine whether IUI might work or whether IVF with ICSI is needed.
Need for investigation: Abnormal results mean further testing is needed—hormones, physical exam, genetic testing, or imaging.
What Semen Analysis Does NOT Tell Us
Here’s where many people get confused:
It doesn’t test sperm DNA quality: Normal-looking, moving sperm can still have DNA damage that prevents fertilization or causes miscarriage. Special DNA tests are needed for this.
It doesn’t measure fertilization ability: Just because sperm look and move normally doesn’t guarantee they can actually fertilize an egg.
It doesn’t predict IVF outcomes reliably: While very abnormal results predict lower success, mildly abnormal results don’t necessarily mean IVF will fail.
It doesn’t assess sperm function: Specialized tests assess whether sperm can actually do what they need to do beyond just looking and moving normally.
It’s a snapshot, not a diagnosis: Sperm production varies a lot. One abnormal result doesn’t mean permanent infertility. WHO recommends at least two tests, 2-3 weeks apart, before drawing conclusions.
It doesn’t explain WHY: The test identifies problems but doesn’t tell you the cause—whether it’s hormonal, genetic, structural, lifestyle-related, or unknown.
The Variability Problem
Results can vary dramatically between samples—even in the same man. Factors that affect results include:
- Days of abstinence
- Fever or illness in the past 2-3 months
- Medications
- Stress and sleep quality
- Season (some studies suggest lower counts in summer)
- Collection method and timing
- Lab techniques
This is why a single abnormal result should never be the basis for major decisions. Always repeat the test.
When Results Are Abnormal
Mild abnormalities (one or two factors slightly off): Repeat test in 2-3 weeks. If consistent, look for treatable causes—varicocele, lifestyle factors, infections.
Moderate abnormalities: Hormone testing, physical exam, possibly genetic testing or ultrasound. Treatment might include medications, surgery, or assisted reproduction.
Severe abnormalities (very low or zero sperm): Comprehensive evaluation including hormone testing, genetic testing, physical exam, and possibly testicular biopsy to see if any sperm production exists.
No sperm at all (azoospermia): Can be a blockage or production failure. Needs specialized evaluation to see if surgical sperm retrieval is possible for IVF with ICSI.
Additional Tests That Might Be Needed
Sperm DNA fragmentation test: Measures genetic damage. High fragmentation (over 30%) is linked to lower fertilization rates and recurrent miscarriage.
Hormone testing: Checks FSH, LH, testosterone, and prolactin to assess hormonal causes.
Anti-sperm antibodies: Tests whether the immune system is attacking sperm.
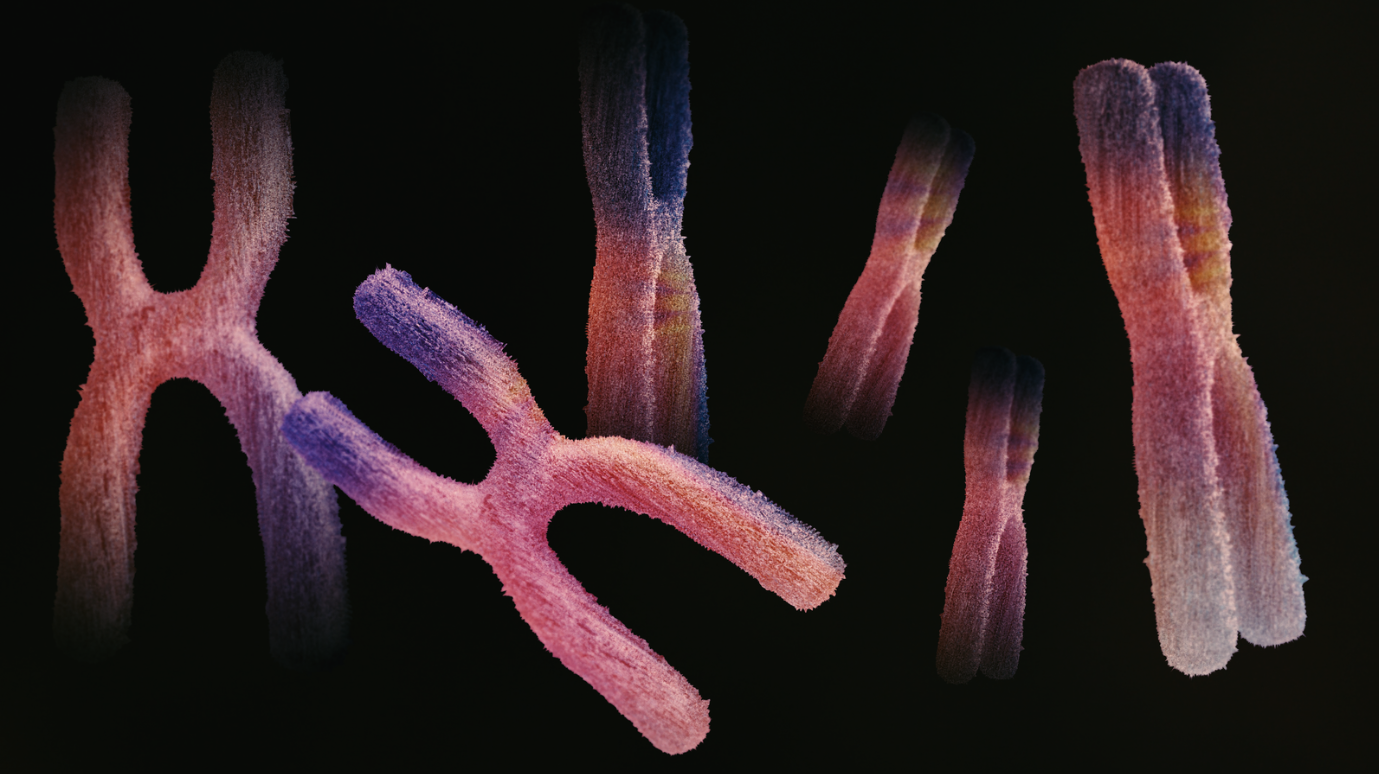
Genetic testing: Checks for chromosomal or genetic problems if counts are very low.
Scrotal ultrasound: Looks for varicocele or structural problems.

Ready to Understand Your Results?
Semen analysis is essential for male fertility evaluation—it’s important, informative, and non-invasive. But it’s just a starting point, not a complete picture.
Normal results don’t guarantee fertility, and mildly abnormal results don’t mean you can’t conceive naturally. The test measures what it can measure, but other aspects of sperm function require additional testing.
If you’re facing abnormal results, remember: sperm production takes 72 days, so today’s results reflect conditions from 2-3 months ago. Many factors affecting sperm can be improved—lifestyle changes, treating infections or varicocele, optimizing hormones—and improvements are possible within a few months.
If you’ve had a semen analysis and have questions about what it means, need guidance on next steps, or want to discuss treatment options, we’re here to help.
Book a consultation to review your results with a specialist who can explain them in context of your overall fertility picture.