Sexually transmitted infections affect fertility pretty significantly. This post breaks it down for you.
Let’s talk about something uncomfortable: sexually transmitted infections and your fertility. Not the easiest conversation to have in a fertility clinic waiting room, or with your doctor, or even with yourself. But here’s the thing—ignoring this topic doesn’t make it go away, and understanding the connection could protect your future family.
If you’re reading this while trying to conceive, or thinking about future children, this information matters more than you might realize.
The Problem Statement
Globally, there are an estimated 374 million new infections annually with one of these four curable STIs: chlamydia, gonorrhea, syphilis, and trichomoniasis.
Here’s what makes this relevant to fertility: untreated STIs in women can lead to pelvic inflammatory disease, infertility, chronic pelvic pain, and pregnancy complications including ectopic pregnancy, early pregnancy loss, stillbirth, and transmission to the baby.
In men, untreated chlamydia and gonorrhea can cause epididymitis—inflammation that can, in rare cases, reduce fertility.
The crucial word here is “untreated.” Because here’s the good news: most bacterial STIs are completely curable with antibiotics. The problem is when people don’t know they have them.
The Silent Problem: No Symptoms
The lesser-known reality: Many cases of gonorrhea and chlamydia have no symptoms at all, especially in women. You can have an infection that’s silently damaging your reproductive system and have absolutely no idea.
This is why screening matters so much. About 10-15% of women with untreated chlamydia will develop pelvic inflammatory disease (PID), and about 1 in 8 women who have had PID have difficulty getting pregnant afterward.
Think about that: you could have a completely symptomless infection today that affects your ability to have children years from now. That’s terrifying, but it’s also preventable.
How STIs Actually Damage Fertility
Let’s break down what’s happening when STIs cause fertility problems:
In Women:
Pelvic Inflammatory Disease (PID): When bacteria from STIs like chlamydia or gonorrhea spread from the vagina and cervix up into the uterus, fallopian tubes, or ovaries, it causes infection and inflammation. This leads to scarring.
Tubal Factor Infertility: Scar tissue in the fallopian tubes can block the path of sperm reaching the egg, or prevent a fertilized egg from reaching the uterus. This accounts for about 30% of female infertility.
Ectopic Pregnancy Risk: Even partial tubing can cause a fertilized egg to implant in the tube instead of the uterus, a dangerous condition requiring emergency treatment.
In Men:
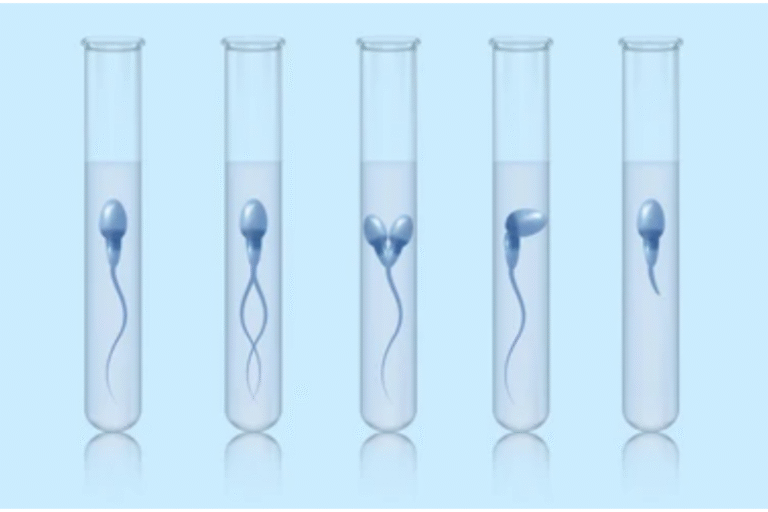
Epididymitis: Chlamydia and gonorrhea can cause inflammation of the epididymis—the coiled tube that stores and carries sperm. If left untreated, this can cause scarring that blocks sperm from being released.
Reduced Sperm Quality: Some studies suggest herpes could potentially affect sperm quantity and quality, though more research is needed.

Who Should Be Tested?
The CDC recommends:
All sexually active women under 25: Annual screening for chlamydia and gonorrhea.
Women over 25: Testing if you have a new partner, multiple partners, a partner diagnosed with an STI, or symptoms.
Men who have sex with men: Screening at least once a year, or every 3-6 months if you have multiple partners.
Anyone experiencing infertility: Ask your doctor about STI testing as part of your fertility workup.
Before trying to conceive: Both partners should consider comprehensive STI screening.
The truth? If you’re sexually active and haven’t been tested recently, you should get tested. There’s no “low-risk” category when it comes to protecting your fertility.
What About Past Infections?
Here’s a question we hear often: “I had chlamydia years ago and got treated. Did it damage my fertility?”
The honest answer: maybe, maybe not. If the infection was caught and treated quickly before it progressed to PID, your fertility is likely unaffected. If you had symptoms of PID (lower abdominal pain, unusual discharge, fever) that went untreated for a while, there’s a possibility of some tubal damage.
The only way to know is through fertility testing—a hysterosalpingogram (HSG) can check if your fallopian tubes are open and clear.
Past infections don’t automatically equal infertility, but they do make fertility evaluation more important if you’re having trouble conceiving.

Prevention and Treatment
Here’s the genuinely hopeful part: bacterial STIs like chlamydia, gonorrhea, syphilis, and trichomoniasis are all completely curable with antibiotics.
Chlamydia: Typically treated with azithromycin (single dose) or doxycycline (7-day course).
Gonorrhea: Usually a single injection plus oral antibiotics.
Syphilis: Penicillin injection.
Trichomoniasis: Metronidazole or tinidazole.
Treatment is straightforward, relatively quick, and highly effective. The key is getting diagnosed and treated before complications develop.
After treatment, you should abstain from sex until you and your partner(s) have completed treatment and any symptoms have resolved. A test of cure is recommended 3-4 weeks after treatment during pregnancy, and testing for reinfection is recommended for everyone three months after treatment.
Prevention: What Actually Works
Condoms: Highly effective at preventing most STIs when used consistently and correctly. Not 100%, but close.
Mutual monogamy: Being in a long-term mutually monogamous relationship with a partner who’s been tested and is uninfected reduces risk dramatically.
Regular testing: Get tested at the start of new relationships, regularly if you have multiple partners, and before trying to conceive.
Partner treatment: If you’re diagnosed with an STI, your partner(s) need treatment too, even if they have no symptoms. Otherwise, you’ll just reinfect each other.
Communication: Talk to partners about sexual health history and testing. Awkward? Yes. Necessary? Absolutely.

The Stigma Problem
Here’s something we need to address: the shame around STIs prevents people from getting tested and treated.
Having an STI doesn’t make you careless, dirty, or irresponsible. STIs are infections—just like any other infection—and they’re incredibly common. Over 1 million STIs are acquired every day globally.
The stigma around STIs is the real problem, not the infections themselves. Most bacterial STIs are easily treatable. The tragedy is when shame prevents people from seeking testing and treatment until permanent damage is done.
If you’re concerned about STIs and fertility, have a history of infections, or just want peace of mind before trying to conceive, we’re here to help. We offer comprehensive STI screening as part of fertility evaluation, in a judgment-free environment.
Book a consultation to discuss testing, treatment if needed, and any concerns about how past or current infections might affect your fertility.
Because protecting your reproductive health isn’t something to be embarrassed about—it’s something to be proactive about.