Implantation is one of the most mysterious processes in all of human reproduction. This blog explains what might be going wrong for you.
You did everything right. You took your medications on schedule, showed up for every monitoring appointment, followed all the instructions. Your embryos looked perfect—beautiful blastocysts that your embryologist described with words like “excellent quality” and “top grade.”
And then they didn’t implant.
The pregnancy test was negative, or maybe it was positive for a brief, heartbreaking moment before the numbers stopped rising. Either way, you’re sitting here wondering: What went wrong? What did I do wrong?
What actually happens during implantation
Before we talk about why implantation fails, let’s understand what needs to go right.
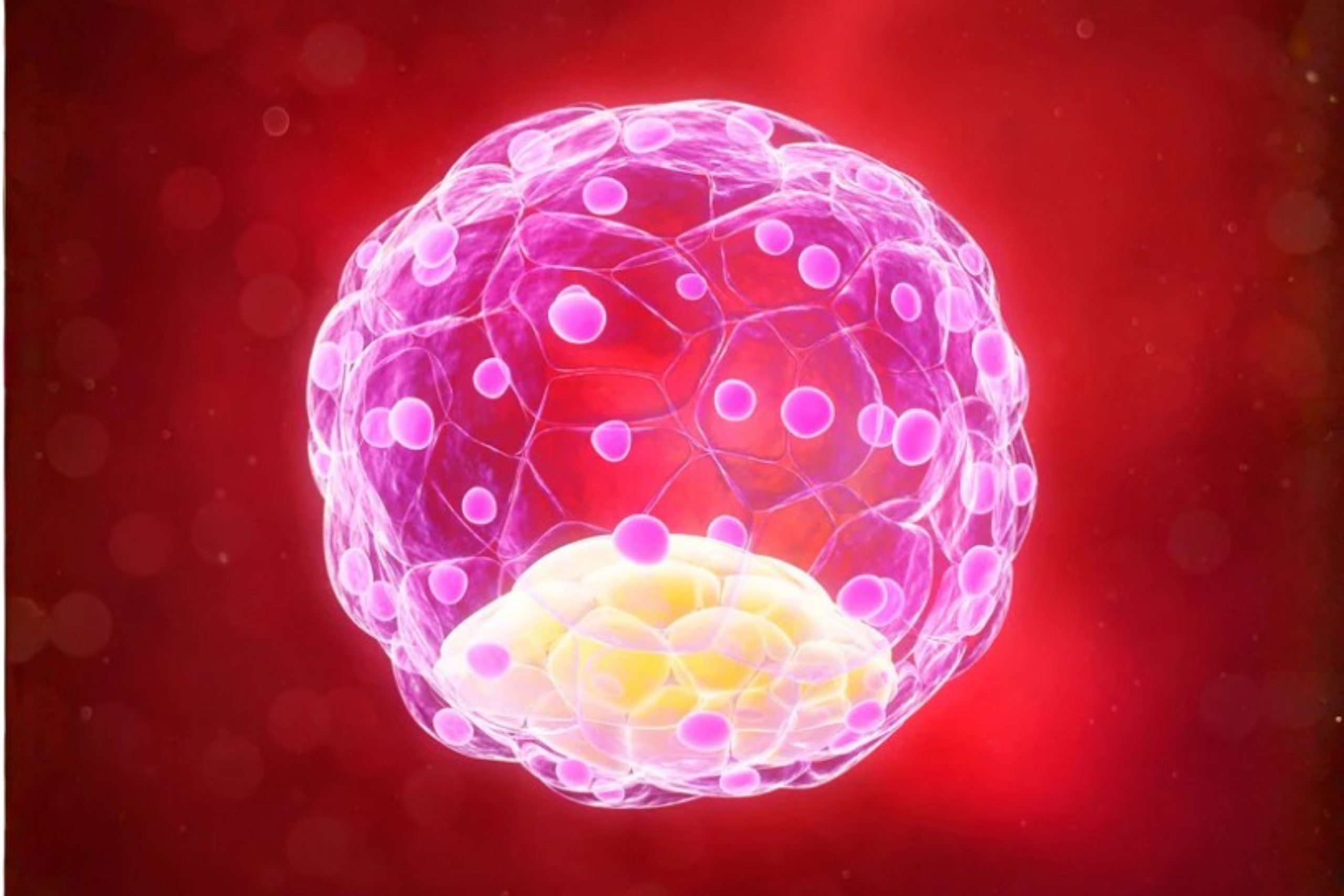
Implantation is the process where your embryo—now a blastocyst, a ball of about 200 cells—attaches itself to the lining of your uterus and begins to burrow in. It happens in three stages:
Apposition: The embryo floats into the right position and makes initial contact with the endometrium.
Adhesion: The embryo sticks to the uterine lining, like Velcro catching hold.
Invasion: The embryo burrows deeper into the endometrial tissue, establishing the connections that will eventually become the placenta.
This entire process requires perfect timing, perfect communication between embryo and endometrium, and hundreds of molecular signals firing in exactly the right sequence. Think of it like two dancers who need to be perfectly in sync—if either one is off by even a beat, the whole performance falls apart.
The Three Main Reasons Embryos Don't Implant
Implantation failure generally comes down to three categories: something about the embryo, something about the uterus, or something systemic in your body. Often, it’s a combination.
1. The Embryo Itself
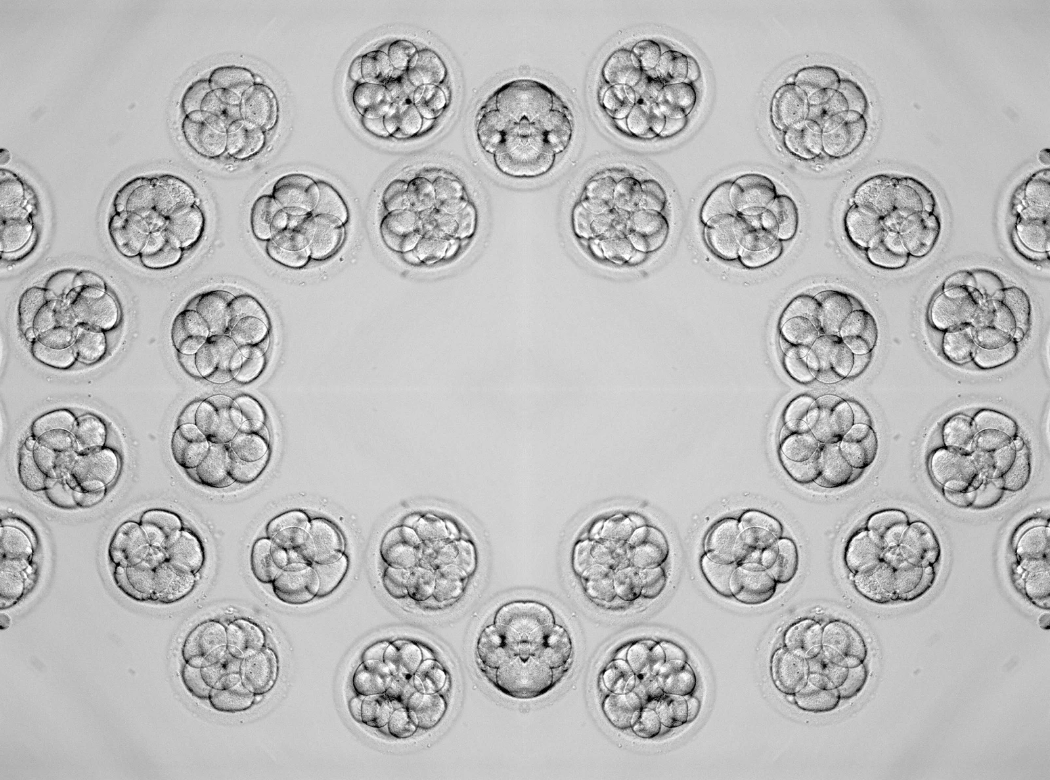
This is the most common reason, and here’s the thing: even beautiful-looking embryos can have hidden problems.
Embryologists grade embryos based on what they can see under a microscope—cell number, symmetry, fragmentation. But they can’t see chromosomes. Research shows that embryo chromosomal status significantly influences implantation ability, and genetically normal (euploid) embryos have much lower rates of implantation failure regardless of maternal age.
The reality is that many embryos—even from young women—have chromosomal abnormalities. These embryos might look perfect, but they’re carrying extra or missing chromosomes that make successful implantation impossible, or if they do implant, they lead to very early miscarriage.
This isn’t something you caused. Chromosomal abnormalities in embryos, including complex abnormalities involving multiple chromosomes, are more common in patients with recurrent implantation failure than in the general population. Some of this is age-related (egg quality declines with age), but some happens randomly even in young, healthy women.
The lesser-known truth: Embryonic mosaicism—where an embryo has a mix of normal and abnormal cells—is actually quite common in human embryos. Some of these mosaic embryos can still implant and result in healthy babies, while others cannot. We’re still learning about which mosaic embryos have potential and which don’t.
2. The Uterus and Endometrium
Even with a perfect embryo, your uterus needs to be ready to receive it. This is where “endometrial receptivity” comes in—a fancy term for whether your uterine lining is actually prepared for implantation at the exact moment the embryo arrives.
Issues that can affect receptivity:
- Thin endometrium: If your lining is less than 7mm thick, implantation becomes much harder. This can happen after D&Cs, with scar tissue (Asherman’s syndrome), or sometimes for unknown reasons.
- Uterine abnormalities: Fibroids (especially if they bulge into the uterine cavity), polyps, adenomyosis, or congenital uterine shape issues can all interfere with implantation.
- Chronic endometritis: A subtle infection or inflammation of the uterine lining that doesn’t cause symptoms but can disrupt the immune environment needed for implantation. Chronic endometritis alters the uterine immune status and may be responsible for impaired endometrial receptivity in recurrent implantation failure.
- Timing problems: The “window of implantation”—that sweet spot when your endometrium is receptive—is different for different women. If your embryo arrives too early or too late, implantation won’t happen. Some women have a shifted window that doesn’t match the standard protocol.
3. Systemic and Immunological Factor
Sometimes the problem isn’t localized to the embryo or uterus—it’s something happening in your whole system.
Causes of recurrent implantation failure can include immunology, thrombophilias (blood clotting disorders), and lifestyle factors. These include:
- Immune factors: Your immune system needs to recognize the embryo as “self” enough not to attack it, but “foreign” enough to trigger the protective immune responses that help pregnancy succeed. When this balance is off, implantation can fail.
- Thrombophilias: Conditions that make your blood clot too easily can affect the tiny blood vessels forming between you and the embryo, disrupting implantation.
- Thyroid dysfunction, diabetes, or other metabolic issues: Hormonal imbalances can affect receptivity even if your lining looks fine on ultrasound.
Lifestyle factors: Obesity (BMI over 30), smoking, and high stress levels have all been associated with higher rates of implantation failure.
Why Age Matters (But Not the Way You Think)
Everyone talks about age and fertility, but here’s the nuance: Age influences both embryo quality and extra-embryonic factors, with older women experiencing reduced embryo implantation even as gestational carriers.
This means two things happen with age:
- Your eggs are more likely to have chromosomal abnormalities (embryo factor)
- Your uterus becomes less receptive to implantation (uterine factor)
But here’s the interesting part: when older women use donor eggs from young women (perfect embryos), their pregnancy rates are much better—but still not as good as young women using their own eggs. This tells us that age affects the uterus too, not just the eggs.

The Frustrating Part: Sometimes We Don't Know Why
Here’s the honest truth that many doctors don’t say clearly enough: sometimes, even after thorough testing, we cannot identify why good embryos aren’t implanting.
You can have A-grade normal looking embryos, a perfect-looking uterus, optimal endometrial thickness, normal hormone levels, and no identifiable immune or clotting issues—and still experience implantation failure.
This is deeply frustrating, we know. Our understanding of implantation is still evolving. There are molecular and cellular processes happening that we can’t yet measure or fully understand.
What can be done about it
The good news is that most couples with implantation failure can eventually achieve pregnancy. The key is systematic investigation and individualized treatment.
Tests that might help identify the problem:
- PGT-A (genetic testing of embryos): To rule out chromosomal issues
- Hysteroscopy: To look inside the uterus for subtle abnormalities, polyps, or scar tissue
- Endometrial receptivity testing (ERA): To check if your window of implantation is shifted
- Thrombophilia panel: Blood tests for clotting disorders
- Immune testing: Though this is controversial and not always helpful
- Chronic endometritis testing: Biopsy to check for hidden infection/inflammation
Treatment approaches that might help:
- PGT-A: Transferring only genetically normal embryos significantly improves implantation rates
- Hysteroscopy with correction: Removing polyps, fibroids, or scar tissue
- Personalized embryo transfer timing: Based on ERA testing results
- Blood thinners: If thrombophilia is identified
- Antibiotics: If chronic endometritis is diagnosed
- Endometrial scratching or PRP: For thin lining (evidence is mixed but may help some patients)
- Immune modulation: In very select cases
The key is that treatment should be based on actual findings, not just throwing everything at the wall to see what sticks.
What You Need to Hear Right Now
If you’re reading this after a failed transfer, here’s what we want you to know:
It’s not your fault. You didn’t think the wrong thoughts, eat the wrong foods, or “stress too much.” Implantation is a biological process that sometimes fails for reasons beyond anyone’s control.
Your embryos being “good quality” doesn’t mean they were guaranteed to work. Embryo grading is based on appearance, not genetics. Even beautiful embryos can carry hidden problems.
Failed implantation doesn’t mean all future attempts will fail. Each transfer is independent. The embryo that didn’t work tells us nothing definitive about the next one.
You deserve answers, but sometimes answers don’t exist yet. Push for thorough testing, but also know that medicine doesn’t have all the answers about implantation. That’s the state of science right now, not a failure of your medical team.
If you’ve experienced failed transfers with good quality embryos, we’re here to help you find answers.
Book a consultation with us to review your history and discuss which investigations make sense for your situation, and create a plan for comprehensive evaluation, including all the tests and treatment options discussed here.
Because you deserve a doctor who takes your implantation failure seriously and has the tools to investigate thoroughly and help you understand what will improve your chances next time, even when the answer is “we’ll try again with what we’ve learned.”